Have you ever wondered what vulva lichen simplex chronicus is and how it affects individuals? This condition, often overlooked, is a persistent form of eczema that specifically targets the vulvar region, causing significant discomfort and affecting the quality of life for those who suffer from it. Many people are unfamiliar with the condition until they or someone they know receives a diagnosis. Understanding the details of this condition is essential for effective management and relief.
Vulva lichen simplex chronicus is characterized by chronic itching and thickening of the skin in the vulvar area, which can lead to a cycle of itching and scratching. This cycle can exacerbate the condition, making it difficult to break free from the discomfort. Patients often experience a diminished quality of life as the symptoms interfere with daily activities, sleep, and intimate relationships. In this article, we will delve deep into the causes, symptoms, treatment options, and ways to manage this condition effectively.
We aim to provide a comprehensive guide that not only educates but also empowers those affected by vulva lichen simplex chronicus. By exploring the underpinnings of this condition, we can offer insights into the latest treatment options and lifestyle adjustments that can help manage symptoms and improve the overall well-being of those affected. Let's embark on this journey to better understand vulva lichen simplex chronicus and explore the avenues for relief and management.
Table of Contents
- Understanding the Condition
- Causes of Vulva Lichen Simplex Chronicus
- Signs and Symptoms
- Diagnosis and Medical Evaluation
- Treatment Options
- Lifestyle Changes and Management
- Psychological Impact and Support
- Common Misconceptions
- Diet and Nutrition
- Alternative and Complementary Therapies
- Importance of Medical Follow-Up
- Living with Vulva Lichen Simplex Chronicus
- Prevention Strategies
- Research and Future Directions
- FAQs
- Conclusion
Understanding the Condition
Vulva lichen simplex chronicus is a skin disorder that primarily affects the vulvar region, causing intense itching and thickening of the skin. It is a chronic condition that can persist for a long time without proper intervention. The condition is classified under the broader category of lichen simplex chronicus, which can occur on various parts of the body but is particularly troublesome when it affects sensitive areas like the vulva.
The condition occurs due to a localized overreaction of the skin to repeated scratching or rubbing, leading to a thickened, leathery texture. This reaction is similar to the body's response to repeated irritation, which can be triggered by various factors such as allergens, stress, or other underlying skin conditions. Individuals with vulva lichen simplex chronicus often find themselves caught in a self-perpetuating cycle where itching leads to scratching, which in turn exacerbates the itching.
Understanding vulva lichen simplex chronicus requires a holistic view of the skin's response to irritation and the psychological factors that may contribute to the condition's persistence. A deeper comprehension of this condition can aid in developing effective treatment strategies and providing relief to those affected.
Causes of Vulva Lichen Simplex Chronicus
The exact cause of vulva lichen simplex chronicus is not completely understood, but it is believed to result from a combination of factors. One of the primary causes is chronic irritation of the vulvar skin, often initiated by an initial trigger such as an allergic reaction or an underlying skin condition like eczema or psoriasis.
Environmental factors also play a significant role in the development of this condition. Exposure to harsh chemicals, synthetic fabrics, or personal care products can irritate the sensitive vulvar skin, leading to an increase in itching and subsequent scratching. Hormonal changes, stress, and emotional factors can further exacerbate the condition, creating a complex interplay of physical and psychological triggers.
Moreover, individuals with a history of atopic dermatitis or other allergic conditions may be more susceptible to developing vulva lichen simplex chronicus. Genetic predisposition can also contribute, as certain individuals may have a heightened skin sensitivity or a tendency to develop skin disorders. Understanding the multifactorial causes of this condition is crucial for identifying effective treatment and management strategies.
Signs and Symptoms
The hallmark symptom of vulva lichen simplex chronicus is intense itching in the vulvar region, which can be severe enough to disrupt daily activities and sleep. This itching is often accompanied by noticeable changes in the skin's texture and appearance. The affected skin may become thickened, leathery, and darker in color, a result of the chronic scratching and rubbing.
Other symptoms include redness, swelling, and the presence of small bumps or lesions on the vulvar skin. Some individuals may also experience burning or soreness, particularly after prolonged scratching. These symptoms can have a significant impact on a person's quality of life, affecting their physical comfort, emotional well-being, and intimate relationships.
In some cases, vulva lichen simplex chronicus may be accompanied by other skin conditions or infections, complicating the diagnosis and treatment process. It is essential for individuals experiencing these symptoms to seek medical evaluation to receive an accurate diagnosis and appropriate treatment plan.
Diagnosis and Medical Evaluation
Diagnosing vulva lichen simplex chronicus typically involves a thorough medical evaluation by a healthcare provider, often a dermatologist or gynecologist. The evaluation process includes a detailed medical history and a physical examination of the affected area to assess the skin's condition and identify any potential triggers or underlying conditions.
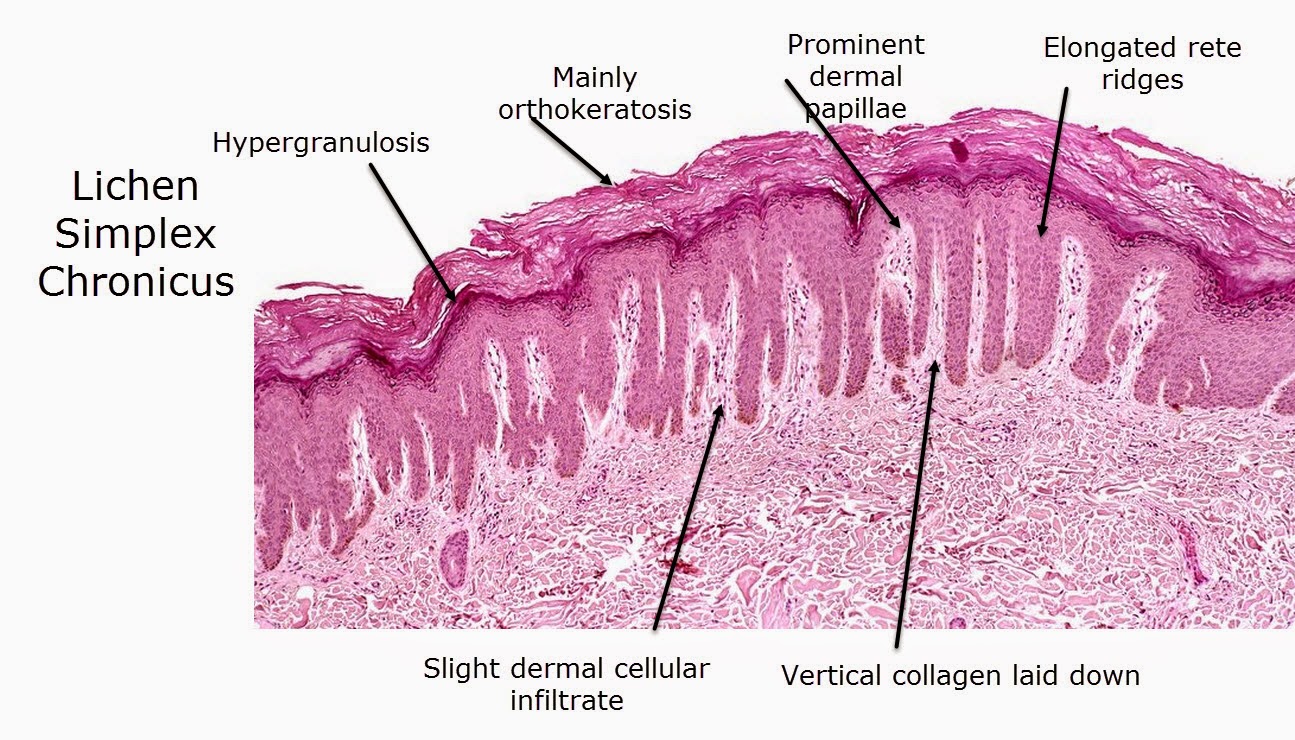
In some cases, a biopsy may be performed to obtain a small sample of skin tissue for analysis. This procedure helps rule out other potential skin disorders and confirm the diagnosis of vulva lichen simplex chronicus. Additional tests, such as allergy testing or blood work, may be conducted to identify any contributing factors or comorbid conditions.
Accurate diagnosis is crucial for developing an effective treatment plan, as the symptoms of vulva lichen simplex chronicus can mimic those of other skin conditions. A comprehensive evaluation ensures that individuals receive appropriate care and management tailored to their specific needs.
Treatment Options
The treatment of vulva lichen simplex chronicus focuses on breaking the cycle of itching and scratching, providing relief from symptoms, and addressing any underlying causes. Topical corticosteroids are often prescribed to reduce inflammation and alleviate itching. These medications are applied directly to the affected area and can provide significant relief when used as directed.
In addition to corticosteroids, other topical treatments such as calcineurin inhibitors or antihistamines may be recommended to manage symptoms. These medications work by modulating the immune response and reducing inflammation in the skin.
Behavioral interventions, such as habit-reversal therapy, can also be beneficial in managing vulva lichen simplex chronicus. These interventions aim to help individuals identify and modify behaviors that contribute to the condition, such as scratching or rubbing, and develop healthier coping mechanisms.
For individuals with severe or persistent symptoms, phototherapy or systemic medications may be considered. These treatments are typically reserved for cases where other interventions have been ineffective and require careful monitoring by a healthcare provider.
Lifestyle Changes and Management
Implementing lifestyle changes is an integral part of managing vulva lichen simplex chronicus. Simple adjustments, such as wearing loose-fitting, breathable clothing made from natural fibers, can help reduce irritation and prevent exacerbation of symptoms. Avoiding harsh soaps, detergents, and personal care products is also essential to protect the sensitive vulvar skin.
Maintaining good hygiene practices, such as gently cleansing the area with mild, fragrance-free cleansers and patting the skin dry, can minimize irritation and promote healing. Moisturizing the skin regularly with hypoallergenic products can help maintain the skin's barrier function and prevent dryness.
Stress management techniques, such as mindfulness, meditation, or yoga, can be beneficial in reducing stress-related triggers and improving overall well-being. By incorporating these lifestyle changes into daily routines, individuals with vulva lichen simplex chronicus can better manage their symptoms and enhance their quality of life.
Psychological Impact and Support
Living with vulva lichen simplex chronicus can have a significant psychological impact on individuals, affecting their emotional well-being and self-esteem. The chronic nature of the condition, coupled with the discomfort and embarrassment of symptoms, can lead to feelings of frustration, anxiety, and depression.
Seeking psychological support from mental health professionals, such as therapists or counselors, can provide valuable coping strategies and emotional support. Support groups or online communities can also offer a sense of connection and understanding, allowing individuals to share their experiences and learn from others facing similar challenges.
Addressing the psychological impact of vulva lichen simplex chronicus is an essential component of comprehensive care, as mental and emotional well-being plays a crucial role in managing the condition and improving quality of life.
Common Misconceptions
Despite being a relatively common condition, vulva lichen simplex chronicus is often surrounded by misconceptions that can hinder understanding and effective management. One common misconception is that the condition is solely a result of poor hygiene, leading to unnecessary stigma and shame for those affected.
Another misconception is that vulva lichen simplex chronicus is a contagious or sexually transmitted condition. This misunderstanding can create unwarranted fear and isolation for individuals, preventing them from seeking appropriate care and support.
It is essential to dispel these misconceptions through education and awareness, promoting a more accurate understanding of the condition and encouraging open dialogue and support for those affected.
Diet and Nutrition
While there is no specific diet for vulva lichen simplex chronicus, maintaining a balanced and nutritious diet can support overall skin health and immune function. Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can provide essential nutrients that promote skin healing and reduce inflammation.
Some individuals may benefit from identifying and avoiding specific food triggers that exacerbate their symptoms. Keeping a food diary and working with a healthcare provider or nutritionist can help identify potential dietary triggers and develop a personalized nutrition plan.
Hydration is also crucial for maintaining skin health, so individuals should aim to drink adequate water throughout the day to support skin hydration and overall well-being.
Alternative and Complementary Therapies
In addition to conventional treatments, some individuals with vulva lichen simplex chronicus may explore alternative and complementary therapies to manage their symptoms. These therapies can include approaches such as acupuncture, herbal remedies, or homeopathy, which aim to address the condition holistically.
While some individuals may find relief through these therapies, it is essential to consult with a healthcare provider before pursuing alternative treatments. This ensures that the chosen therapies are safe, appropriate, and do not interfere with conventional treatments.
Incorporating alternative and complementary therapies into a comprehensive treatment plan can provide additional support and symptom relief for those with vulva lichen simplex chronicus.
Importance of Medical Follow-Up
Regular medical follow-up is crucial for individuals with vulva lichen simplex chronicus to monitor the condition's progression and ensure the effectiveness of the treatment plan. Follow-up appointments allow healthcare providers to assess the skin's response to treatment, make necessary adjustments, and address any new or persistent symptoms.
Ongoing communication with healthcare providers is essential for managing vulva lichen simplex chronicus effectively, as it allows for timely intervention and support. Individuals should feel empowered to discuss any concerns or questions with their healthcare team, ensuring that their care is comprehensive and individualized.
Living with Vulva Lichen Simplex Chronicus
Living with vulva lichen simplex chronicus requires a proactive approach to symptom management and self-care. By incorporating treatment strategies, lifestyle changes, and supportive measures, individuals can effectively manage their symptoms and improve their quality of life.
Building a strong support network, whether through healthcare providers, support groups, or loved ones, can provide valuable encouragement and assistance. Staying informed about the latest research and treatment options empowers individuals to make informed decisions about their care and take an active role in managing their condition.
With the right support and resources, individuals with vulva lichen simplex chronicus can navigate the challenges of the condition and lead fulfilling, healthy lives.
Prevention Strategies
Preventing vulva lichen simplex chronicus involves minimizing exposure to potential triggers and maintaining good skin care practices. Avoiding irritants such as harsh soaps, synthetic fabrics, and perfumed products can reduce the risk of developing or exacerbating the condition.
Paying attention to skin care and hygiene practices, such as using gentle cleansers and moisturizers, can help maintain the skin's barrier function and prevent dryness and irritation. Managing stress through relaxation techniques, exercise, or therapy can also reduce stress-related triggers and support overall well-being.
By implementing these prevention strategies, individuals can reduce their risk of developing vulva lichen simplex chronicus and maintain healthy, comfortable skin.
Research and Future Directions
Ongoing research into vulva lichen simplex chronicus aims to improve understanding of the condition's underlying mechanisms and develop more effective treatment options. Advances in dermatology and immunology research hold the potential to uncover new therapeutic targets and strategies for managing the condition.
Future research directions may include exploring the role of the immune system, genetic factors, and environmental influences in the development and progression of vulva lichen simplex chronicus. Collaborative efforts between researchers, clinicians, and patient advocacy groups can drive progress and innovation in the field.
By staying informed about the latest research and developments, individuals with vulva lichen simplex chronicus can access cutting-edge treatments and interventions that enhance their quality of life.
FAQs
- What is vulva lichen simplex chronicus?
Vulva lichen simplex chronicus is a chronic skin condition affecting the vulvar region, characterized by intense itching and skin thickening due to repeated scratching or rubbing.
- What causes vulva lichen simplex chronicus?
The condition is caused by a combination of factors including chronic irritation, allergic reactions, environmental triggers, hormonal changes, and stress.
- How is vulva lichen simplex chronicus diagnosed?
Diagnosis involves a medical evaluation by a healthcare provider, often including a physical examination, medical history review, and sometimes a skin biopsy.
- What treatments are available for vulva lichen simplex chronicus?
Treatment options include topical corticosteroids, other topical medications, behavioral interventions, and in some cases, phototherapy or systemic medications.
- Can lifestyle changes help manage the condition?
Yes, lifestyle changes such as wearing loose clothing, avoiding irritants, practicing good hygiene, and managing stress can help manage symptoms and improve quality of life.
- Is vulva lichen simplex chronicus a contagious condition?
No, vulva lichen simplex chronicus is not contagious or sexually transmitted. It is a skin disorder resulting from chronic irritation and other factors.
Conclusion
Vulva lichen simplex chronicus is a challenging condition that requires comprehensive management to alleviate symptoms and improve quality of life. By understanding the causes, symptoms, and treatment options, individuals can take proactive steps to manage their condition effectively. With the support of healthcare providers, lifestyle changes, and ongoing research, those affected by vulva lichen simplex chronicus can navigate the challenges of the condition and lead fulfilling lives.
By staying informed and empowered, individuals can advocate for their health and well-being, ensuring that they receive the care and support they need to thrive. As research continues to advance, new treatments and interventions will offer hope and relief for those living with vulva lichen simplex chronicus.
You Might Also Like
Discover The Best Take Out Food In Fremont, CA: A Culinary JourneyUnderstanding Electric Bike Street Legal Regulations: A Comprehensive Guide
Munwex.com: A Comprehensive Guide To Understanding Its Impact And Opportunities
Unleashing The Magic Of Adopt Me Codes March 2024: Your Ultimate Guide
Water Houses In Minecraft: Building Your Aquatic Dream Home
Article Recommendations
- Sharknado 4 The Fourth Awakens
- Walker Shepard
- Decimal Form Of 1 3
- Enoch In Spanish
- Blue Hanfu
- How To Put Mba On Resume
- Cheryl Hines
- Cold Steak
- Barron Trump Gay
- How Many Siblings Did Elvis Presley Have